Date: 8th March 2022
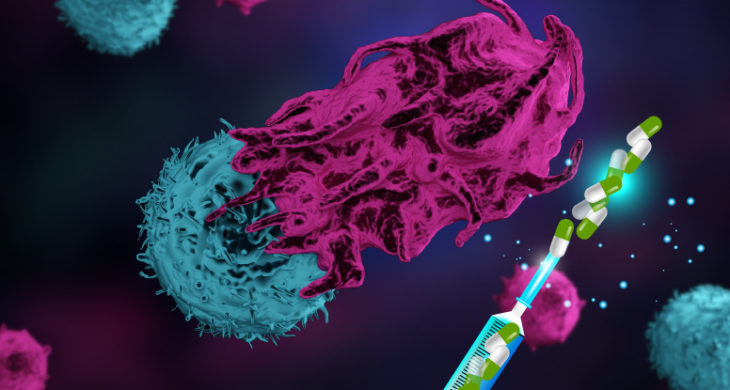
Cytokines are major regulators of the innate and adaptive immunity and activate disease fighting immune cascades in the body. Cytokine therapy has been used to activate the immune system of cancer patients and is an important treatment modality in the clinic. Interleukin-2 (IL2) has been a source of interest for immuno-oncology as it plays a critical role in the regulation of T cells, and its use in melanoma and renal cancer has already been approved by the Food and Drug Administration (FDA). However, IL2 has a very short half-life in blood meaning high-dose infusion regimes are required to achieve tumour reduction, the knock on effect is a high level of off-target effects and often severe toxicity in many patients. Now, researchers have developed a clinically translatable cytokine delivery platform composed of polymer-encapsulated human ARPE-19 (RPE) cells that produce natural cytokines. An IL2-producing cytokine factory treatment eradicated peritoneal tumours in ovarian and colorectal mouse models in as little as 6 days.
A major challenge in the field of immunotherapy is to increase tumour inflammation and anti-tumour immunity while avoiding systemic side effects of cytokines and other pro-inflammatory drugs. Attempts to improve cytokine therapy by improving recombinant protein safety and pharmacokinetics have been made following advances in protein engineering and controlled release formulations. However, finding an approach that simultaneously addresses short lifetime, maintains full biological activity and limits systemic toxicity has remained elusive for many, including IL2.
Now, researchers at Rice University, US, led by Omid Veiseh, have shown they can eradicate advanced-stage ovarian and colorectal cancer in mice in as little as six days with an implantable bead-like ‘drug factory’ which delivered continuous, high doses of IL2 at the tumour site, in a treatment that could be ready for human clinical trials later this year.
The team started by engineering human retinal pigmented epithelial (RPE) cells to stably express a proinflammatory cytokine of choice including human IL2. The engineered cells were then encapsulated within alginate-based microparticles (capsules), cells remained viable after encapsulation, did not divide, produced the cytokine of interest and survived longer in vivo that cells not encapsulated.
The team wanted to assess whether the cytokine factories allowed for spatial and temporal control of cytokine delivery in mice. They reasoned that capsules implanted within the intraperitoneal (IP) cavity would create high cytokine concentrations within the IP cavity while maintaining low concentrations in the blood, as it is separated from the systemic circulation. Furthermore, cancers which frequently metastasise often do so to the peritoneal cavity. 100 capsules were implanted into the IP cavity and produced at least 30x higher local concentration of cytokine than in the systemic concentration.
The team were also able to control the dosing by varying the amount of capsules per dose, and by giving multiple doses. The local IP concentration increased with the number of capsules delivered, and cytokine levels in the IP fluid were consistently more than 100x higher than in the blood. Crucially, expression was consistent across mice in each group, demonstrating the robustness of the platform to tightly control cytokine production.
Next, the team tested the cytokine factories for tumour eradication. In a mouse model of advanced ovarian cancer, 100-200 implanted capsules reduced tumour burden within 6 days, and by day 30 100% of mice showed a reduction in tumours, the highest dose (200 capsules) had 147× less tumour burden. Further analysis showed that the treatment induced cytotoxic T cell proliferation, this was essential for the antitumour response, and experiments in mice which lacked fully functional T and B cells showed that tumour ablation post treatment no longer occurred in these immune-deficient mice.
A similar tumour reduction was seen in under a week for colorectal cancer. Four of five mice were tumour free by day 15 after injection and remained so until the end of the experiment 57 days later. Re-challenge experiments also showed that the treatment aided the development of memory T cells that prevent secondary tumours from developing.
A key design consideration for the hIL2 cytokine factory was their clinical translatability – with all the individual components of the system being previously proven safe for use in humans. The team performed several translatability and safety tests in nonhuman primates showing a profile predictive of human efficacy and that the treatment was well tolerated and showed few sign of toxicity.
Conclusions and future applications
The team here have designed a modular cytokine factory for therapeutic use, consisting of microencapsulated cells that can be used for local in vivo delivery of mono- as well as combination therapies. The results here are supportive of translation into human clinical trials for ovarian and colorectal cancers, and offer a safe and predictable method to treat cancer.
One of the strengths of this method is the design. All components have previously been tested and deemed safe in human, the team hope this will translate to a quick transmission in to clinic trials, which they are aiming for later this year.
One key feature of the system is the ability to switch off the therapy once completed. Here the team exploited the natural foreign body response (FBR) to immunostimutaory hydrogel particles. This caused pericapsular fibrotic overgrowth (PFO) on the alginate capsule’s surface, over time decreasing the pore size, and eventually leading to cell death upon depletion of oxygen and nutrients. PFO was witnessed in both models by day 14, and by then the cells inside the capsule were no longer detected, demonstrating efficient switching off. The precise control of IP therapeutic concentrations is a unique feature of the encapsulated cell therapy platform, which is qualitatively not achievable by biologic injections.
The cytokine factory technology will provide the field with an invaluable tool that can be easily modified and leveraged for other peritoneal cancers such as renal, liver, pancreatic, and cervical cancers in future clinical studies and could enable further exploration of therapeutics with substantial toxicity at narrow concentration windows where they are both safe and effective. Avenge Bio, a Massachusetts-based startup co-founded by Veiseh, has licensed the cytokine-factory technology from Rice University.
Other advances recently made in cytokine therapy are now starting to be applied in clinical trials. Researchers have demonstrated that intratumoural administration of saline-formulated messenger (m)RNA encoding four cytokines promoted antitumour immunity and tumour eradication across multiple preclinical cancer models and have entered clinical trials. Immunocytokines – engineered antibody-cytokine protein fusions- are also showing promise in a pilot trial in patients for glioblastoma. However, the spatial, temporal and tunable control of the cytokine factories will be a most valued property of this system. What is clear from all of these technologies is the expanding repertoire of immunotherapies offers great hope for overcoming refractory and intractable cancers in the very near future.
Furthermore, cytokine therapy is not just restricted to treating cancer, and for example it has recently been used to reverse paralysis by nerve cell regeneration. Such work is also likely to benefit from advanced delivery systems such as cytokine factories.
For more information please see the press release at Rice University
Ghani, S., Joshi, I., Isa, D., et al. (2022). Clinically translatable cytokine delivery platform for eradication of intraperitoneal tumors. Science Advances 8, eabm1032.
https://doi.org/10.1126/sciadv.abm1032
http://eha.3a7.mywebsitetransfer.com/mrna-cytokine-therapy-eradicates-tumours-enters-clinical-trials/
http://eha.3a7.mywebsitetransfer.com/new-immunocytokine-therapy-shows-promise-glioblastoma/
http://eha.3a7.mywebsitetransfer.com/designer-cytokine-reverses-paralysis-by-nerve-cell-regeneration/