Date: 21st October 2021
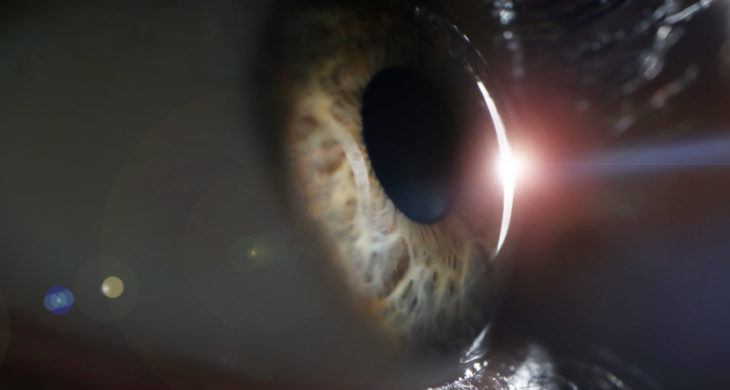
Glaucoma is a progressive neurodegenerative disease which to date has no cure. It affects over 60 million people worldwide, leaving 8 million blind. It is the most common cause of blindness in people over 60 years old however, it does not just afflict the elderly, as it can also be present at birth as primary congenital glaucoma. For infants surgery is the preferred therapy, but for all, current therapies are supportive and focused on the reduction of intraocular pressure (IOP), a primary risk factor for glaucoma progression. Now, scientists use a new, long-lasting protein treatment to replace the function of mutated glaucoma causing genes, preventing the formation of the condition in a primary congenital glaucoma model, and which shows promise as a potential therapy in adults.
Primary congenital glaucoma (PCG) is a severe disease characterised by developmental defects in the trabecular meshwork (TM) and Schlemm’s canal (SC), comprising the conventional aqueous humour outflow pathway of the eye. The angiopoietin (ANGPT)-TEK (tunica interna endothelial cell kinase) system is an endothelial growth factor pathway comprised of the receptor tyrosine kinase TEK, which is highly expressed by SC endothelial cells, and its ligands, the angiopoietins. Recent works have shown a link between PCG in children and heterozygous loss of function variants in TEK or its primary ligand ANGPT1, or compound variants in TEK/SVEP1. Furthermore, ANGPT1 and ANGPT2 have been associated with primary open-angle glaucoma (POAG) in adults. The pathway is an essential regulator of IOP homeostasis and inhibition can cause ocular hypertension, together these data suggest this pathway may be a potential therapeutic target for glaucoma.
Now, scientists at Northwestern University Feinberg School of Medicine, US, led by Susan Quaggin, have shown that tissue-specific deletion of Angpt1 or Svep1 caused PCG in mice. Delivery of a recombinant ANGPT1-mimetic promoted developmental SC expansion in healthy and Angpt1 deficient eyes, blunted intraocular pressure (IOP) elevation and RGC loss in a mouse model of PCG and lowered IOP in healthy adult mice.
Using gene editing, the team developed new models of glaucoma in mice that resembled PCG. Tissue-specific depletion of Angpt1 or Svep1 in the neural crest tissue of mice, caused severe defects in the SC, exhibited ocular hypertension and had a similar phenotypes to PCG.
To further categorise distinct TM and SC cell populations and to discover additional TM-SC signalling pathways the team performed single-cell transcriptomic analysis of normal and the glaucomatous Angpt1 deficient eyes. They identified a population of putative SC endothelial and TM cells, and were able to catalogue sets of genes of interest for future glaucoma studies. However, the essential nature of the ANGPT-TEK signalling in SC development remained strong.
This led the team to hypothesise this pathway might be a valuable target for glaucoma therapy aimed at increasing SC function and outflow through the conventional route, thereby reducing IOP. They had previously developed a highly effective soluble ANGPT1-mimetic fusion protein which they now used to treat healthy and glaucomic eyes.
Wild type mice at birth were injected with the fusion protein, which led to a dramatic increase in SC area and lowered IOP. Furthermore, when the mimetic protein was injected in to the PCG-model mice the treatment was sufficient to partially rescue SC development and IOP was lowered even after treatment has ceased, suggesting this may represent a good strategy for treating glaucoma.
Whilst PCG is totally devastating, it only represents a small percentage of glaucoma sufferers, so next the team wanted to determine whether this new fusion protein treatment was a viable option for adult patients. 24 h after bilateral intravitreal injection in adult animals, a marked reduction in IOP was observed in the mimetic treated group compared to the control animals, suggesting this treatment would translate well for more commonly occurring glaucoma.
Conclusions and future applications
The work here has demonstrated the importance of TM-SC crosstalk and confirmed that TM-expressed molecules are essential drivers of SC development and function. By deriving new models of PCG the team have shown that a soluble ANGPT1-mimetic protein promoted developmental SC expansion in both healthy and PCG-eyes, lowering IOP significantly without pathological angiogenesis.
In addition, the team have catalogued several other signalling molecules in the single-cell transcriptomics dataset which have been implicated in glaucoma and offer exciting opportunities for future studies and drug development directly targeting the conventional outflow pathway.
The team are hoping that the work here will lead to the first targeted therapy that effectively promotes (aqueous humour) fluid outflow from the front of an eye, reversing the underlying biologic defect in patients with glaucoma.
This work should add to the growing and diverse new set of tools that are aimed not only at restoring sight due to glaucoma but from other types diseases. Recently, scientists have used gene therapy to deliver an adapter molecule, Protrudin, into the eye which stimulated axon regeneration of the damaged nerve fibres, and protected them from cell death after injury, offering hope of a new treatment for glaucoma. Other gene therapy has been used to deliver a highly photosensitive protein into retina bipolar cells bypassing degenerative photoreceptors and restoring vision in blind mice modelled for age related macular degeneration.
In vivo gene editing has been explored to treat a rare eye condition Leber congenital amaurosis and has already reached the clinic, being recently approved by the US Food and Drug Administration. Interestingly, unilateral gene therapy has unexpectedly improved vision in both eyes as a result of Leber hereditary optic neuropathy, which may have profound implications for gene therapy clinical trial design and outcome measures. Lastly, new technologies such as digital health platform which can read IOP via an injectable sensor may be an invaluable tool to assess and monitor the success of treatments such as these. As such this new wave of therapies and applications are set to change the traditional and currently limited way in which we treat sight loss, and offers to change the lives of millions of patients, and it is hoped restore sight to many.
For more information please see the press release at Northwestern University
Thomson, B.R., Liu, P., Onay, T., Du, J., Tompson, S.W., Misener, S., Purohit, R.R., Young, T.L., Jin, J., and Quaggin, S.E. (2021). Cellular crosstalk regulates the aqueous humor outflow pathway and provides new targets for glaucoma therapies. Nature Communications 12, 6072.
https://doi.org/10.1038/s41467-021-26346-0