Date: 25th November 2020
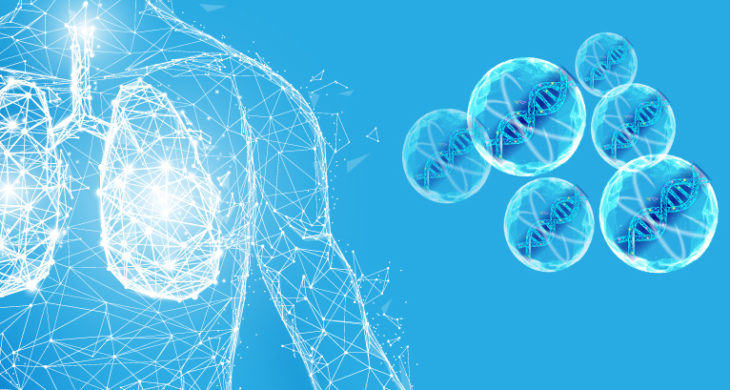
Cystic fibrosis (CF) is an autosomal recessive genetic disorder, and there are currently more than 70,000 people living with the disease worldwide. CF is associated with thick and hyperviscous mucus which accumulates in various organs and is particularly damaging in the lungs. Now, scientists have used lipid nanoparticles loaded with engineered mutated mRNA, which acts as an ion channel inhibitor, ameliorating mucous dehydration in CF, and offering a new potential therapeutic for all CF patients.
CF results from a plethora of mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene. CFTR regulates epithelial sodium channel (ENaC) activity in the airways, which becomes dysregulated in CF patients. This leads to excessive water absorption due to unopposed ENaC activity, which results in dehydrated airway surface liquid (ASL), which then impairs ciliary motion. ENaC is a heterotrimeric channel which is composed of three subunits – α, β, and γ – and the α-ENaC subunit is essential in forming a functional channel.
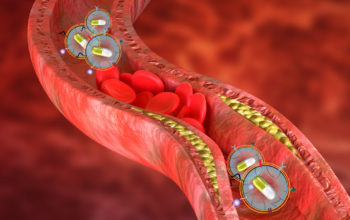
Now scientists led by Gaurav Sahay, from Oregon Health & Science University, US, have inhibited endogenous ENaC channels by introducing an inactivating mutant ENaC α mRNA (αmutENaC), packaged in a lipid nanoparticle (LNP), and delivered intranasally to CF-modelled mice, where it inhibited sodium and water reabsorption activity.
The team started by formulating the LNPs using four lipids, and used them to encapsulate mRNA which encoded for a mutated version of the α subunit, αmutENaC. The mutations were designed to prevent the excision of an 8-mer imbedded inhibitory peptide in the subunit, which when released, is critical for ENaC activation. The team hypothesised that the exogenous mutated subunit would compete with the endogenous α and δ subunits and would form inactivated channels with a low open probability.
To test the system in vitro the team first transfected the αmutENaC in airway cells – created from the bronchial epithelium of a CF homozygous patient. They showed that the resultant mutant protein was expressed 72 hours post transfection, and that the short-circuit currents (ISC) of the αmutENaC-transfected cells were significantly lower that the control cells, without compromising cell viability.
Normally, the ASL lines the mucosal surface of the airway cells, aiding clearance by the cilia. However, in CF patients the height of the ASL is reduced due to dehydration, which impairs the mucociliary clearance. To investigate this further the researchers measured ASL height in the CF-airways cell. They found that the reduction of ENaC activity in the αmutENaC-transfected cells led to an increase in the ASL height, likely due to a decrease in mucosal Na+ and water hyperabsorption.
In vivo CF-mice model testing
As the in vitro data was promising the team wanted to test the therapy in a more clinically relevant model, so they used a CFTR knockout mouse. Initial experiments showed that intranasal administration of a reporter mRNA – LNP resulted in expression of the cargo in the nasal epithelium 5 hours post delivery, suggesting the delivery system was viable. So the team then went on to evaluate the αmutENaC mRNA-LNPs.
Nasal potential difference is used to measure the voltage across the nasal epithelium, which results from transepithelial ion transport and is commonly used as an in vivo diagnostic and research tool as it in part reflects CFTR function and can substitute for measurements of electrophysiological activities of the lower airways. The team therefore, took NPD measurements from control and αmutENaC mRNA–LNP transfected CFTR null mice.
The team observed an increase in NPD in the CFTR null mice, suggesting elevated ENaC activity compared with wild type mice. Intranasal delivery of αmutENaC mRNA–LNP over two consecutive days resulted in a decrease of this NPD – signifying that ENaC activity was inhibited, this then rose back to the original-elevated levels after 2 weeks, likely due to clearance of the exogenous mutant mRNA by this time.
Conclusions and future applications
Unopposed or excessive ENaC channel activity is a long-standing proposed mechanism in CF pathophysiology. The team here, have shown that a new mRNA therapeutic – αmutENaC mRNA–LNP – can decrease and inhibit ENaC activity, ameliorating some of the phenotypes associated with CF.
Whilst, the team showed their mRNA therapy could increase the ASL height in CF- airway cell lines by 34%, they have yet to show whether this was enough to increase ciliary beat frequency, which would be essential to restore function. This is an area of research they will be studying in the future and how this translates into re-establishing cilia function in vivo has yet to be determined.
The power of this potential therapeutic is that it is universal to CF patients. Gene therapies or gene editing therapies are becoming an increasingly popular method being explored to treat a range of diseases and disorders such as Duchenne muscular dystrophy, muscular dystrophy or to restore sight or hearing to name just a few. However, many of these require the precise repair of individual mutations, or delivery of large genes. Scientists have found more than 1,700 different mutations in the CFTR gene, and have being trying for over 30 years to design effective gene therapies against CF. Whilst, new technologies are accelerating this work, the large volume and range of mutations combined with lack of effective targeted delivery systems means this has remained a challenge. With this new mRNA therapy comes the hope of a potentially universal treatment of CF, regardless of underlying CFTR mutations.
However, there are still many hurdles to overcome before this therapeutic translates to the clinic. A key challenge the team will need to address is how to deliver the therapy through the characteristic thick, viscous mucous in the airways of CF patients. Nanoparticles coated with non–mucus-adhesive polymers have already been shown to readily penetrate CF sputum and will be investigated further.
The team hope that mRNA-based ENaC inhibition will become a powerful strategy for reducing mucus dehydration and will translate into a therapeutic for treating all CF patients, independent of genotype, and will greatly improve patient lives and life expectancy.
Mukherjee, A., K. D. MacDonald, J. Kim, M. I. Henderson, Y. Eygeris and G. Sahay (2020). “Engineered mutant α-ENaC subunit mRNA delivered by lipid nanoparticles reduces amiloride currents in cystic fibrosis–based cell and mice models.” Science Advances 6(47): eabc5911.
https://doi.org/10.1126/sciadv.abc5911