Date: 22nd January 2021
Spinal cord injury (SCI) is damage to the spinal cord that causes temporary or permanent changes in its function, often causing severe and permanent disabilities due to the lack of regenerative capabilities of the severed axons. Now, scientists report significant locomotor recovery of both hindlimbs after a complete spinal cord crush using gene therapy to deliver a potent designer cytokine.
Spinal cord injuries resulting from sports or traffic accidents often causes permanent disabilities such as paraplegia. The central nervous system (CNS) is refractory to regeneration and therefore, severed axons are unable to repair. Attempts to stimulate axon regeneration have produced limited success, and as such there are currently no cures available for SCI in the clinic. However, one area that has seen recent success is axon regeneration in the optic nerve of the eye.
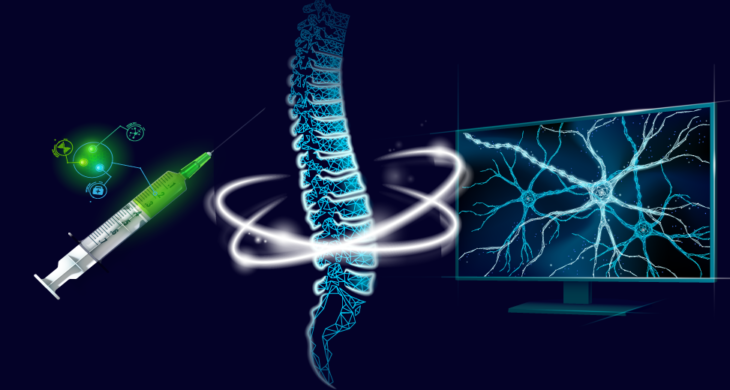
Now, researchers led by Dietmar Fischer, from Ruhr University of Bochum, Germany, have built on their previous work which used gene therapy to deliver the designer cytokine hyper-interleukin-6 (hIL-6) to stimulate optic nerve regeneration after injury. Here, they transduce cortical motoneurons with an adenoviral vector (AAV) expressing hIL-6, which stimulated regeneration of neurons in the deep brain stem, and restored hind limb movement after paralysis from a complete spinal cord crush injury.
The activation of the Janus kinase/signal transducer and activator of transcription 3 (JAK/STAT3) pathway can stimulate the regeneration of CNS axon in the optic nerve, and is therefore a candidate pathway for stimulating axon regeneration in other parts of the body. However, whilst interleukin-6 (IL-6) type cytokines, such as IL-6 itself, are activators of the JAK/STAT3 pathway, the cytokine-specific α-receptor subunits in CNS neurons that are required for signal induction are only expressed at low and restricted levels.
In order to overcome these limitations, the team previously engineered a designer cytokine, hIL-6, which consisted of the bioactive part of the IL-6 protein covalently linked to the soluble IL-6 receptor α subunit, meaning that this synthesised cytokine could directly bind to the signal-transducing receptor subunit glycoprotein 130 (GP130) which is abundantly expressed by almost all neurons.
Using hIL-6, the researchers wanted to test whether AAV delivery of this designer cytokine could affect corticospinal tract (CST) regeneration following complete spinal cord crush (SCC). So the team adminstered a one-time unilateral application of AAV-hIL-6 into the sensorimotor cortex, at 7 weeks after birth, straight after the SCC was performed.
The treatment promoted axon regeneration, and restored many aspects of locomotion in as little as 2-3 weeks. It restored plantar stepping with full hindlimb weight support, followed by lift-off, forward limb advancement, and reestablishment of weight support at initial contact in most of the animals. Meanwhile, the control animals only showed active ankle movements which included spasms.
Interestingly, despite only administering a unilateral treatment, both limb movements improved. Furthermore, bilateral injection did not improve movement beyond that already observed. More detailed work then determined that the transduced hIL-6 could stimulate the neurons trans-synaptically, by releasing the protein at the axon terminals.
Conclusion and future applications
The team here have shown a one-time, unilateral application of AAV2-hIL-6 gene therapy into the sensorimotor cortex significantly improved functional recovery after a complete SCI in adult mammals. It promoted axon regeneration in the neurons located in brain regions that are challenging to access but relevant for functional recovery after spinal cord injury.
The team are now looking to address whether other activators or suppressors of the JAK/STAT3 pathway can enhance or are detrimental to hIL-6 promoted regeneration, with an aim to optimise the effects.
Further experiments are also planned to explore and extend a time window of treatment. Here, the treatment was administered immediately after injury however, in the clinic any treatment given would be hours or even days after injury. How this would impact the efficacy of AAV hIL-6 therapy is as yet unclear.
The work here represents an exciting step forward in finding new approaches for treating spinal cord injuries. By repurposing previous work in axon regeneration in the optic nerve, the team have potentially found an approach with cross – injury applications. With this is mind, it should be noted that others have also stimulated optic nerve regeneration. We recently reported the use of gene therapy to deliver an adapter molecule, Protrudin, into the eye which stimulated axon regeneration of the damaged nerve fibres, and protected them from cell death after injury, offering hope of a new treatment for glaucoma. Whether other approaches of stimulating axon regeneration are transferable to spinal cord injuries is yet to be tested.
Whilst, this study is still in its infancy, finding novel therapies will be crucial for treating such injuries or diseases that affect the CNS. The ability to stimulate neuron regeneration will open up new avenues for treatments which will hopefully translate into the clinic in the near future.
For more information please see the press release from Ruhr University of Bochum
Leibinger, M., C. Zeitler, P. Gobrecht, A. Andreadaki, G. Gisselmann and D. Fischer (2021). “Transneuronal delivery of hyper-interleukin-6 enables functional recovery after severe spinal cord injury in mice.” Nature Communications 12(1): 391.
https://doi.org/10.1038/s41467-020-20112-4