Date: 25th February 2021
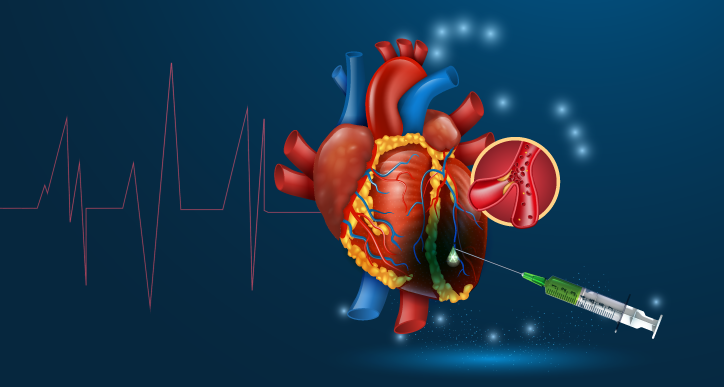
Ischaemic heart disease is the leading cause of mortality worldwide, accounting for 16% of the world’s total deaths. It induces the necrosis of millions of cardiomyocytes, leading to acute inflammation, abnormal remodelling of the extracellular matrix (ECM), scarring, and ultimately to heart failure. Now, scientists have created an extracellular matrix (ECM)–mimicking hydrogel which reduced fibrosis, increased angiogenesis, and led to a complete functional recovery of ejection fraction after myocardial infarction.
The ECM network plays a crucial role in cardiac homeostasis and it contains components that modulate the ischemic microenvironment. Both the composition and mechanical properties of the ECM undergo changes in diseased hearts and therefore it has been an area of extensive research as a route for disease treatment.
Now, researchers from the National University of Ireland Galway, Ireland, the University of Milano-Bicocca, Italy, University Paris Est, France, University of Gothenburg, Sweden, and the University of Valladolid, Spain, led by Abhay Pandit have used synthetic recombinantly produced polypeptides that mimic natural elastin, called elastin-like recombinamers (ELRs), to produce a hydrogel that was sensitive to cleavage by matrix metalloproteases after myocardial infarction (MI). In a sheep model for a common form of MI, injection of the hydrogel led to a significant positive histological, biological and functional recovery of the injured heart muscle.
The team started by synthesising the ECM-inspired responsive ELRs-hydrogel. The first ELR was sensitive to proteases which are normally expressed after MI, the second ELR contained cell adhesion domains. The two ELRs were then cross-linked, forming a hydrogel that was porous and therefore capable of allowing cell colonisation and then post-ischemic remodelling.
Next, the team wanted to establish a new clinically relevant, large animal model for non-transmural MI (NSTEMI), which does not involve the full thickness of the wall of the heart. This is now the most common clinical form of MI, but there is currently lack of suitable research models. The team induced the infarct by multiple ligations in an ovine model, and then 7 days later injected the ELRs-hydrogel via intramyocardial injection.
They found that injection of the degradable ELRs-hydrogel improved cardiac function and limited fibrosis during post-ischemic remodelling. Only in the ELRs-treated group did the average decrease in ejection fraction due to the MI completely reverse, showing an average improvement of ~16% at 21 days post treatment. The fibrotic region was decreased by ~44% in this group, and had ~ 51% less collagen fibres, this was also accompanied by a decrease in proinflammatory markers.
Next, the team wanted to assess post-ischemic remodelling after treatment. They showed that ELRs-hydrogel acted as scaffold, allowing different types of stromal cells to invade the hydrogel and migrate through it. There was also an increase in angiogenesis potential seen by endothelial cell sprouting.
Whilst, these improvement were beneficial would it have an effect on cardiomyocyte survival? Here, the team found pathway analysis data suggested a possible effect on cell survival mechanisms. In support of this, there were more GATA4+ cardiomyocytes in the infarct border zone of ELRs-hydrogel treated hearts. GATA4 is a cardiac transcription factor associated with cellular survival, and also has anti-apoptotic effects. Furthermore, the infarcted wall thickness was significantly lower in the control groups, suggesting a return to muscular thickness in the ELR-treated hearts. Overall, the data suggested that the ELRs-hydrogel limited intracellular damage of the cardiomyocytes.
Conclusions and future applications
The team here have demonstrated the functional benefits that ELRs-hydrogels have in a clinically relevant MI model. It highlights the potential for such treatments for clinical translation which the team will be pursuing further.
One consideration is the timely delivery and route of administration for the ELRs-hydrogel. Here, open-chest delivery of treatment was performed, which is widely accepted in research models. The investigation into alternative methods of delivery in the clinic may offer further advantages and increase the range of patients able to receive such treatment, as surgery is high risk and not always required. However, as a many patients undergo coronary artery bypass surgery after this type of MI, the ELRs-hydrogel injection could be given at the same time.
It is hoped that this work will add to the innovative and novel therapies that are currently being developed for coronary vascular disease and those being designed to greatly improve outcomes after MI. We have seen the likes of base-editing being used to treat coronary disease or biohijacking of macrophages to deliver drugs for the treatment of atherosclerosis. The generation of an acellular hydrogel, as is the case for ELRs-hydrogel, offers several advantages as they are easily synthesised, easily adapted or personalised, and don’t carry the risks of introducing immunogenic cells or cell parts. Recent work on a new cell free therapy using exosomes has been shown to regenerate heart tissue and improve recovery from MI. It is hoped that the ELRs-hydrogel will offers the promise of cardiomyocyte preservation and restoration of cardiac function, and will progress towards clinical trials in the future.
For more information please see the press release from National University of Ireland Galway
Contessotto, P., D. Orbanić, M. Da Costa, C. Jin, P. Owens, S. Chantepie, C. Chinello, J. Newell, F. Magni, D. Papy-Garcia, N. G. Karlsson, M. Kilcoyne, P. Dockery, J. C. Rodríguez-Cabello and A. Pandit (2021). “Elastin-like recombinamers-based hydrogel modulates post-ischemic remodeling in a non-transmural myocardial infarction in sheep.” Science Translational Medicine 13(581): eaaz5380.
https://doi.org/10.1126/scitranslmed.aaz5380