Date: 5th March 2021
The apolipoprotein E gene (APOE) is the most highly validated genetic risk factor for late-onset Alzheimer’s disease (AD) and for many other diseases such as cardiovascular diseases. The human APOE gene has 3 common variants, and the ɛ4 allele (APOE4) is carried by almost half of Alzheimer’s patients. Whilst, it has been implicated in AD pathogenesis as a modulator of multiple pathways, including lipid transport and metabolism, its mechanism of action is largely unknown. Now, researchers show that APOE4 disrupts lipid homeostasis in astrocytes, and have identified genetic and chemical modulators of this lipid disruption, treatment with one –choline- was able to restore cellular lipidome to its basal state.
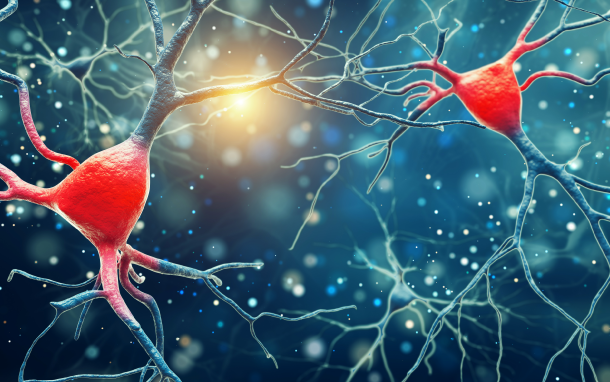
Astrocytes are the most abundant glial subtype in the central nervous system (CNS), and similar to microglia, they play a crucial role in the regulation of neuroinflammation. Microglia become progressively activated and seemingly dysfunctional with age, and accumulation of lipids in glia is a pathologically defining feature of AD.
APOE encodes a lipid-carrier proteins that is a key component of many lipoprotein particles, and acts as a ligand for membrane receptors that mediate lipoprotein uptake. The presence of APOE4 decreases the onset age of AD and increases the lifetime risk for developing the disease in a gene dose-dependent manner.
Now, scientists led by the late Susan Lindquist, former director of MIT’s Whitehead Institute for Biomedical Research, and Li-Huei Tsai at Massachusetts Institute of Technology, US, have shown that human induced pluripotent stem cell (iPSC)–derived astrocytes generated from APOE4, but not APOE3, displayed cellular lipidome disruption. Genetic screens in yeast, revealed that choline supplementation to promote phospholipid synthesis, restored normal lipid state in both APOE4-expressing yeast and human astrocytes.
To start the team wanted to determine the impact of the APOE4 variant allele on astrocytes, as they are the major source of APOE in the brain. They compared the lipid composition of human iPSC-derived APOE4-expressing astrocytes to APOE3-expressing human iPSC-derived astrocytes and found there was a large increase in triacylglycerides in the APOE4-astrocytes. Further investigations revealed these astrocytes had accumulated a greater number of lipid droplets, and the associated lipid-droplet-resident protein, Perilipin-2, compared with their APOE3 counterparts.
These results suggested an intracellular lipid dysregulation by APOE4 in astrocytes but would other cells involved in AD behave in a similar manner? To answer this the team looked at microglia, which also accumulate lipids with age. Once again they saw APOE4-expressing microglia displayed an increased lipid droplet numbers per cell over time when compared with APOE3-microglia, although these cells were not as susceptible under the same conditions as the astrocytes.

Lipid metabolism in the human cortex
Interestingly, these observation were substantiated in transcriptomic data from post mortem human brain tissue, which carried the APOE4 allele. Genes associated with metabolism of neutral lipids and cholesterol were up-regulated, and those involved with fatty acid metabolism and other neutral lipids were down-regulated, suggesting APOE4 also regulates lipid metabolism in vivo in the human cortex.
Yeast genetic screens
Next, the team exploited the yeast system as a genetically tractable platform as there is significant conservation of lipid metabolism pathways across eukaryotes. Here, the expression of APOE4 in yeast recapitulated lipid defects identified in the human astrocytes, and was accompanied by a specific growth defect. To identify genetic suppressors of the APOE4-induced phenotype the team performed loss-of-function genetic screens, with the restoration of the growth phenotype a readout of candidates involved in the process. They found, that the enriched genes were those encoding proteins that regulate lipid metabolism, act as sensors for fatty acid saturation or phospholipid composition confirming APOE4’s role in lipid metabolism.
Cellular lipid metabolism is influence not only by genes but also by the environment. Therefore, the team hypothesised that by changing the medium composition they could restore lipid homeostasis in yeast, in an effort to identify a potential therapeutic. Using their top genetic screen hit, OP1, a negative regulator of phospholipid synthesis, they tested whether ethanolamine or choline which are soluble precursors of phospholipid synthesis could supplement growth. Indeed, choline salts added to the yeast medium reversed the yeast growth defects and lipid dysfunction due to APOE4, decreasing intracellular triacylglycerides and unsaturated fatty acids attached to them.
Choline supplements also restored defective lipid homeostasis in the human APOE4-expressing iPSC-derived astrocytes and rescued cholesterol accumulation that was also observed in the these astrocytes.
Conclusions and future applications
The team here have demonstrated that APOE4 has a central role in perturbing lipid metabolism pathways, which can be rescued by the supplementation of choline. As APOE4 is a significant risk factor for AD, APOE4-associated diseases have been linked to alterations in glucose and fatty acid metabolism, and the human APOE4-expressing cortex showed dysregulation of lipid metabolism, modulation of glial metabolism could play a crucial role in protecting against neurodegenerative diseases such as AD.
Looking to the future the team will expand their findings to more clinically relevant in vitro models, and they will determine whether restoration of lipid homeostasis can ameliorate AD symptoms. They hope to determine whether dietary changes can affect the brain metabolites and lipids in both animal models and human carriers of APOE4. Such research could identify early-stage markers that could be used to identify APOE4-dependent pathological states. As choline is a readily available supplement and has already been tested in clinical trials, their use to halt or restore genotype-specific glial lipid homeostasis would be a relatively easy translation.
Worldwide, ~50 million people are living with dementia, and AD is the most common – contributing to 60-70% of cases. With no cure or ways to stop or slow its progression, current medications merely treats the symptoms.
As such there is a great unmet clinical need for therapies and medication that address disease progression. Inroads are being made however, such as the launch of Neuroglee Therapeutics who are attacking AD through personalised AI-powered digital therapeutics. Recent work using artificial intelligence has identified maternal autobodies as a diagnostic biomarkers of autism, as several of the autoantibodies studied have also been proposed as biomarkers for Alzheimer’s disease this may translate as an early risk indicator, prior to the appearance of disease symptoms. Scientists are also developing nanoparticle platforms to deliver inhibitory molecules to ablate the expression of key neurodegenerative players. This is in response to traumatic brain injury, but as these types of injuries are associated with AD it may act as an effective pre-emptive tool.
The addition, of the work here in laying the framework for manipulating lipid metabolism as a therapeutic approach for those carrying the APOE4 allele will hopefully translate to an effective yet simple way to alleviate or halt the progression of AD symptoms in the near future. It will open up new avenues for AD research and accelerate novel therapeutic strategies.
For more information please see the press release from the Massachusetts Institute of Technology
Sienski, G., P. Narayan, J. M. Bonner, N. Kory, S. Boland, A. A. Arczewska, W. T. Ralvenius, L. Akay, E. Lockshin, L. He, B. Milo, A. Graziosi, V. Baru, C. A. Lewis, M. Kellis, D. M. Sabatini, L.-H. Tsai and S. Lindquist (2021). “<em>APOE4</em> disrupts intracellular lipid homeostasis in human iPSC-derived glia.” Science Translational Medicine 13(583): eaaz4564.
https://doi.org/10.1126/scitranslmed.aaz4564