Date: 5th October 2021
There are just under 500,000 new cases of pancreatic cancer diagnosed every year. Compared with many other cancers, the combined five-year survival rate for pancreatic cancer is very low at just 5-10%. Poor outcomes for pancreatic cancer are due to the fact it metastasises and quickly spreads, and patients often present late, meaning it is usually incurable. Now, researchers have engineered a ‘time machine’ - a lifelike reproduction of a pancreatic structure called the acinus – which they’ve used to show how to reverse the course of cancer before it spreads throughout the pancreas.
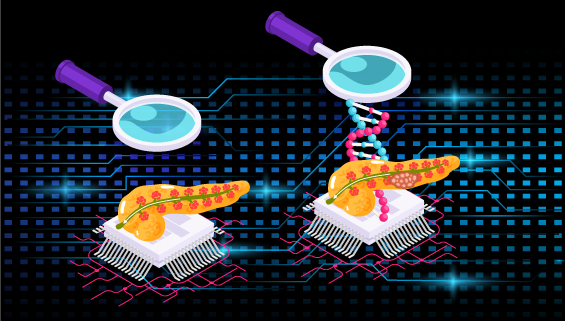
Researchers typically investigate future disease or cancer treatments in animal models, but whilst this is an essential part of the drug development process it can take months for cancer models to develop in an animal. Advanced in the field of nanotechnology and bioengineering have led to the development of miniaturised devices such as lab-on-a-chip or organ-on-a-chip and offer us new ways to study cancer development and treatment concepts in a realistic way. They accelerate research, saving time and money as high-throughput and automation become a possibility, and they give scientists far more control over the model. However, from an engineering perspective creating the anatomical complexity of in vivo structures is extremely challenging and has been limiting to date.
Now, engineers at Purdue University, US, led by Han Bumsoo, have developed an in vitro model of the acinus, named pancreatic acinus-on-chip (PAC), akin to a ‘time machine’. Using PAC the team have shown that reprogramming with a gene essential for normal pancreas development, PTF1a, can convert pancreatic cancer cells back to a more normal and differentiation acinar phenotype, essentially reversing the cancer phenotype.
A pancreatic acinus is a functional unit of the exocrine pancreas producing and secreting digestive enzymes. Its pathobiology is crucial to pancreatic diseases including pancreatitis and pancreatic cancer, which can initiate from pancreatic acini. To create the PAC, the researchers developed the model as a microfluid platform, recreating the cavity-filled acinus and the duct, which is also involved in the spread of pancreatic cancer. The epithelial duct and acinar sac geometry were microfabricated by a newly developed two-step controlled ‘viscous-fingering’ technique – where a more viscous fluid displaces a less viscous fluid.
Using a glass platform on a microscope slide the team created two interconnecting chambers. A collagen solution was loaded into one chamber creating the finger-like shape of the pancreatic duct, which then bulged and expanded into the second chamber creating the cavity of the acinus. To study the cancer, human pancreatic cells were then loaded into the acinus chamber.
For years, Stephen Konieczny, author of the study and professor at Purdue, had studied the gene PTF1a, which is critical for normal pancreas development. The team hypothesised that PFT1a might be a ‘reset’ button, where re-activation of gene expression in cancer cells could revert the cells back to a normal phenotype.
To address this, the team engineered a pancreatic cancer cell line with an inducible (doxycline) PTF1a gene and placed them into the PAC. Once the gene was activated, the cells started constructing the rest of acinus, indicating they were no longer cancerous, and they forming a structure akin to those found in vivo. Further bioinformatic analyses suggested that, the cells had transitioned into a more normal and differentiated acinar phenotype.
Conclusions and future applications
The team here have built a realistic in vitro model of pancreas structures that are involved in pancreatic cancer pathology, that acts as a time machine to study and understand cancer progression and can act as a testbed for potential treatments and therapies. Here, they show that pancreatic cancer cells can be reprogrammed by induction of PTF1a expression, reverting the cells back into a normal state and phenotype.
These findings open up new avenues for designing and testing new gene therapies or drugs. Indeed, Han’s lab is currently conducting experiments using PAC to explore a possible gene therapy. It is the first time, the normal three-dimensional (3D) architecture of the acinus has been seen in vitro, and mimics healthy tissue. This will likely translate to a useful platform to study other diseases and conditions of the pancreas.
This work will add to the ongoing efforts to develop new tools for cancer research such as recent work where 3D-bioprinted tumour models of glioblastoma were supported by perfusable blood-like vessels, or patient-derived lung cancer organoids that can predict patient therapeutic responses with 100% accuracy. These new modelling approaches are starting to emerge as faithful recapitulators of in vivo tumours, showing similar growth curves, drug response, and genetic signatures. Together these applications are providing ground-breaking platforms that can potentially replace animal models, at least partly, and offer to accelerate the development of new drugs and therapies, in addition to enabling must faster predictions of the best treatments for patients.
For more information please see the press release at Purdue University
Venis, S.M., Moon, H.-r., Yang, Y., Utturkar, S.M., Konieczny, S.F., and Han, B. (2021). Engineering of a functional pancreatic acinus with reprogrammed cancer cells by induced PTF1a expression. Lab on a Chip 21, 3675-3685.
https://doi.org/10.1039/D1LC00350J

