Date: 23rd November 2021
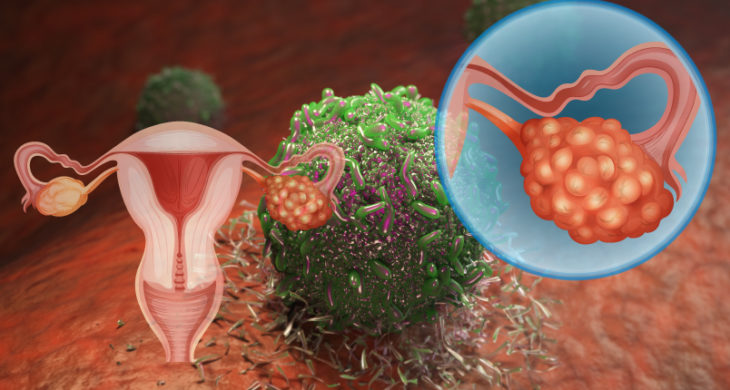
Immune checkpoint inhibitors (ICI) are a type of cancer treatment that help T cells recognise and attack tumours. Whilst the introduction of ICI therapy has revolutionised cancer care, even the in the most responsive of cancer types, only a minority of patients (20-40%) respond to single-agent ICIs. In other cancer types the response can be disappointingly low, for example the ICI response rate in patients with ovarian cancer is only favourable in 10-15% upon single-agent ICI. Now, researchers reveal that cancer-associated mesenchymal stem cells (CA-MSCs) drive immunotherapy resistance by immune exclusion, and targeting Hedgehog (HH) signalling improved tumour responses to immunotherapy.
A tumour microenvironment (TME) is thought to dictate responses to ICI, and patients with an immune-infiltrated molecular signature have a better prognosis compared to patients with a desmoplastic/mesenchymal signature. Desmoplasia - the growth of fibrous or connective tissue- and intratumoural fibrosis drives resistant to treatments, and work has shown that resistant ICI-tumours are also associated with activation of the HH pathway. Another player of interest in the desmoplastic and immune response are MSCs although their involvement in cancer is currently unclear, and in particular their role in antitumour immunity in epithelial tumours, such as ovarian cancer, has remained mechanistically undefined.
Now, researchers at the University of Pittsburgh and University of Pittsburgh Medical Center, US, led by Ronald Buckanovich, have demonstrated that CA-MSCs induced CD8+ T cell tumour immune exclusion and inhibited response to ICI, which was mediated by recruitment of myeloid cells. Inhibition of HH signalling reduced tumour-associated monocytes and macrophages, reversing T cell immune exclusion, increasing natural killer (NK) cells into the TME which ultimately led to restoring tumour responsiveness to a common immunotherapy, anti-PD-L1 (Programmed death-ligand 1).
To start the team assessed the impact of CA-MSCs on the tumour immune microenvironment in a chemotherapy resistant model of ovarian cancer in mice. Tumour cells alone or mixed with CA-MSCs were injected subcutaneously and whilst the control tumour were highly infiltrated by CD8+ T cells, tumours cell mixed with CA-MSCs showed immune exclusion, with the T cells being restricted to areas of peritumoral desmoplasia. Furthermore, tumour-associated macrophages (TAMs) which have been shown to reduce T cell motility and limit their trafficking into tumour islets were increased, suggesting a mechanism for the drive towards immune exclusion.
Next, the team used this model to evaluate the impact of CA-MSCs on the therapeutic efficacy of anti–PD-L1 immune therapy. The control mice with tumours all succumbed to cancer, but ~50% of those treated with anti–PD-L1 injections had their tumours eradicated. Meanwhile, the cohort that had received tumour/CA-MSC mixed, revealed that anti–PD-L1 treatment had no impact on increasing overall survival thereby demonstrating that CA-MSCs inhibited the response to anti–PD-L1 checkpoint immunotherapy. They also determined that the effect was mediated by recruitment of myeloid cells that expressed high levels of TGF-β induced (Tgfbi), and that this and other immune cell recruitment activity could be inhibited by several neutralising antibodies against key immunosuppressive cytokines.
The team had previously shown that HH inhibitors (HHis) could reverse CA-MSC–driven desmoplasia and resistance to chemotherapy so the next question was whether HHi could similarly affect CA-MSC immune function. To address this, they started in vitro using a U.S. Food and Drug Administration–approved HHi agent, demonstrating this agent did not enhance the response to anti–PD-L1 treatment in tumours lacking CA-MSCs but specifically did enhance the response for those in the presence of CA-MSCs, in addition to restoring CD8+ T cell infiltration in these tumours.
But how would this translate in vivo? Here the team showed that HH inhibition combined with anti–PD-L1 reduced the Tgfbi+ myeloid cells and increased NK cell presence in tumours, and restored the response to ICI therapy. Together, these data implicate CA-MSCs as regulators of antitumor immunity, and that CA-MSC hedgehog signalling is an important target for cancer immunotherapy.
Conclusions and future applications
The team have demonstrated that CA-MSCs are a critical driver of the immune-suppressive TME and an important therapeutic target to overcome resistance to ICI therapy in ovarian cancer. They have identified potential therapeutic targets – such as Tgfbi – which was found to predict a poor response to immunotherapy. These discoveries will open new avenues for treating immunotherapy-resistant ovarian cancer.
Indeed, with this in mind the researchers have partnered with Genentech, who will provide the HHi. They are planning to launch a new clinical trial early next year, to determine whether HHi can improve the benefits of immunotherapy in patients with therapy-resistant ovarian cancer. They are hoping this approach will have significant benefit for these patients, and that it will offer new treatment options for the patients that currently have very few.
Finding methods to circumvent immune resistance will be a highly valuable tool for oncologists and the work detailed here will add to a growing body of work aimed at turning ‘cold’ tumours into ‘hot’ one. For example researchers have identified other key molecules - such as DDR1 - that prevent immune cells from entering aggressive breast cancer tumours, and that its depletion can halt tumour growth and protect against future tumours. These types of approaches of making tumours accessible to immune cells will hope to increase the efficacy of immunotherapies for a range of cancers, and provide better patient outcomes for those that currently have limited treatment options.
For more information please see the press release at UPMC
Osmanbeyoglu, H.U., et al. (2021). Cancer-associated MSC drive tumor immune exclusion and resistance to immunotherapy, which can be overcome by Hedgehog inhibition. Science Advances 7, eabi5790.
https://doi.org/10.1126/sciadv.abi5790