Date: 15th March 2022
Duchenne muscular dystrophy (DMD) is a genetic disorder characterised by progressive muscle degeneration and weakness due to the alterations of a protein, dystrophin, that helps keep muscle cells intact. Frameshift mutations in the DMD gene, cause this terminal disease, and as it is located on the X-chromosome it primarily affects males. It is estimated ~20,000 children are diagnosed with Duchenne globally every year, typically patients lose their ability to walk, and develop heart and lung complications as they age. Currently, treatments for DMD are limited, and there is no known cure, whilst existing therapies can slow the time it takes for symptoms to take hold, these however are particularly ineffective in treating weakened heart muscles. Now, researchers show in a Phase II clinical trial that a cellular therapy is safe and effective in stopping the deterioration of upper limb and heart functions, and is the first treatment to lead to meaningful functional improvements in the most severe cases of DMD patients.
The HOPE-2 clinical trial was performed at UC Davis Health and six other sites in the US, and enrolled late-stage DMD patients aged 10 years or older with moderate upper limb impairment. It was designed to examine the safety and efficacy of sequential intravenous infusions of Capricor Therapeutics’ CAP-1002 allogeneic cardiosphere-derived cells (CDCs) obtained from human heart muscles.
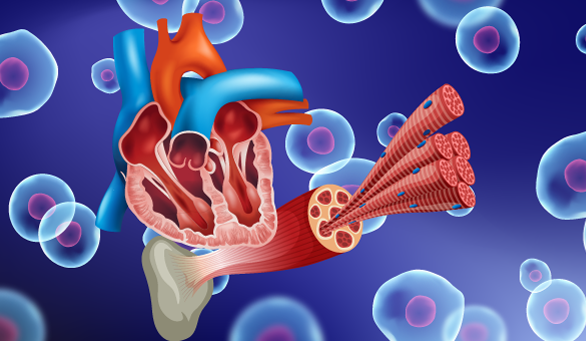
Cardiac-derived cell therapy was first identified in the laboratory of Eduardo Marbán, scientific founder of Capricor, and has been shown in pre-clinical and clinical studies to exert potent immunomodulatory activity. CDCs are currently being investigated for their potential to modify the immune system’s activity to encourage cellular regeneration. Exosomes released by CDCs are taken up by macrophages and T cells and begin a cycle of repair, altering their expression profile so they adopt healing rather than proinflammatory phenotypes. Along with immunomodulatory properties they also exhibit antifibrotic, and regenerative properties, and confer disease-modifying bioactivity in models of Duchenne muscular dystrophy.
The trial is the first with repeat sequential dosing of cells for a genetic illness. Eight patients received the CAP-1002 therapy whilst the rest received a placebo, the cell therapy was administered intravenously once every 3 months for a total of 4 infusions. The team assessed upper limb function using the scale Performance of Upper Limb (PUL) motor function for DMD. They found a clinically significant 71% slowing of loss of function in the treated group at the 12-month milestone.
They also tested heart function using cardiac magnetic resonance imaging (MRI). Whilst, the placebo group showed significant decrease in left ventricular ejection fraction (LVEF), a global measure of cardiac pump function, the CAP-1002 cohort improved slightly, overall a 107% slowing of loss of heart function at 12 months. The structure of the heart also showed signs of improvement.
Overall, the therapy was well tolerated although infusion-related hypersensitivity reactions were observed in 3 patients, without long-term consequences. One patient had to discontinue the therapy due to a severe allergic reaction.
Conclusions and future applications
The team here have shown that CAP-1002 cell therapy appears to be safe and effective in reducing deterioration of upper limb function in patients with late-stage DMD, and also improved heart function and structure.
Longer-term extension studies will be needed to confirm the therapeutic durability and safety of CAP-1002 beyond 12 months. The team will also be launching a Phase III clinical trial, which will confirm the efficacy of CAP-1002 in a larger cohort of patients. This will be the next milestone towards gaining drug approval with the FDA.
Whilst, this is cell therapy is unique in that it addresses both cardiac and upper limb deterioration, it is also the first to focus on non-ambulatory patients. If successful in Phase III of the trial, the cell therapy will offer hope to the least mobile patients with the greatest unmet needs.
Researchers around the world are also investigating the use of CRISPR gene editing to alleviate DMD symptoms. It has been shown that somatic CRISPR gene editing in living pigs can restore the DMD reading frame, resulting in expression of a shortened but largely functional dystrophin protein. This led to widespread dystrophin expression in muscle, including in the diaphragm and heart, resulting in prolonged survival and reduced arrhythmogenic vulnerability.
At present, several therapeutic companies are working on CRISPR programmes for DMD, such as Vertex Pharmaceuticals, CRISPR Therapeutics and Sarepta Therapeutics. Whilst, these potentially offer a single-treatment permanent ‘cure’, there are many challenges to this approach. DMD is caused by many mutations meaning multiple different gene-editing programmes may have to be investigated. Efficient systemic delivery of gene-editing cargo at required therapeutic levels is problematic, particularly for the heart. Damage already done by the disease may not be reversed by this method, so the best outcomes will be achieved with the earliest possible treatment, although recent advances such as the CRISPR-Chip, which is able to detect mutations associated with DMD, will aid early diagnosis. Furthermore, these strategies are currently still in discovery or preclinical stages and are therefore still a significant time away from reaching the market. Whilst the development of therapies to treat early-stage DMD such as CRISPR-based approaches will be an important strategy, the ability to treat DMD after the onset of symptoms such as here with CAP-1002 will be a valuable options for many patients.
It is hoped that CAP-1002 will make a tremendous impact on the quality of life for boys and young men with DMD in the near future, addressing the later stages of the disease, allowing them to perform manual tasks that relate to daily living, and lessen the burden of care for their families.
For more inf0ormation please see the press release at UC Davis Health or at Capricor
McDonald, C.M., Marbán, E., Hendrix, S., Hogan, N., Ruckdeschel Smith, R., Eagle, M., Finkel, R.S., Tian, C., Janas, J., Harmelink, M.M., et al. (2022). Repeated intravenous cardiosphere-derived cell therapy in late-stage Duchenne muscular dystrophy (HOPE-2): a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. The Lancet 399, 1049-1058.
https://doi.org/10.1016/S0140-6736(22)00012-5
http://eha.3a7.mywebsitetransfer.com/crispr-gene-editing-relieves-duchene-muscular-dystrophy-symptoms/
http://eha.3a7.mywebsitetransfer.com/crispr-chip-biosensor-detects-unamplified-dna/