Date: 17th November 2020
Regulatory T cells (Tregs) are modulators of the innate and adaptive immune response to both foreign and self-antigens, and can help suppress undesirable immune responses. As such they have great therapeutic potential for a variety of conditions such as autoimmune diseases, graft-versus-host disease and transplantation rejection. However, translation into the clinic has been hampered by poor in vivo homeostasis of the adoptively transferred Tregs, and they become quickly absent from the circulation. Now, scientists have developed a new drug delivery platform, which can be engineered to autostimulate Tregs with nanogel ‘backpacks’ delivering interleukin-2 (IL-2) under certain conditions, allowing alloimmunity suppression in mouse and humanised models of skin transplantations.
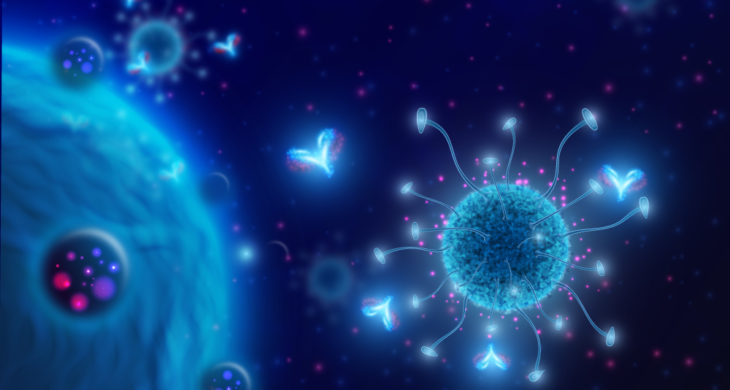
A key success factor for a potential Tregs therapy is the maintenance of immunosuppressive qualities which requires continuous T cell receptor (TCR) ligation and a permissive environment that delivers exogenously produced factor IL-2. Strategies that deliver a low systemic dose of IL-2 have been tried but can also lead to the activation of other proinflammatory cells such as cytotoxic T lymphocytes and natural killer (NK) cells, causing adverse therapeutic outcomes.
Now, an international team scientists led by Jamil Azzi and Darrell Irvine, from the Harvard Medical School and Massachusetts Institute of Technology, US, have designed a TCR signalling–responsive cytokine-delivery platform for Tregs that delivers IL-2 via nanoparticle backpacks, activating these cells at sites of antigen encounter, and suppressing alloimmunity in mice.
The team had previously demonstrated a method to create TCR-signalling responsive backpacks for tumour specific T cells, consisting of protein nanogels loaded with an IL family member. In general, once T cells and Tregs, are stimulated and become antigenically primed, reducing agents in the cytoplasm and cell surface are upregulated, which counters the oxidative stress. The backpacks reacted to this, and released their cargo in response to these heightened redox potential, enabling spatiotemporal control of adjuvant discharge.
The team therefore, hypothesised they could functionalise adoptive Treg with IL-2 loaded-backpacks to suppress alloimmunity – an immune response to non-self antigens from members of the same species, which often occurs during graft-versus-host disease and is the major cause of transplantation rejection.
To start, the team surface engineered Tregs with the backpacks by conjugating them to the surface membrane of the cells (NG Tregs). The cells despite the backpacks remained phenotypically unchanged however, survival of the cells was increased in vitro. Importantly, the team didn’t observe any off target effects on other T cells, implying that the IL-2 was consumed by the backpack cells, and that it did not spill over to the neighbouring cells, which can cause cytotoxic cell activation.
In vivo suppression
With encouraging in vitro results the team want to test the in vivo suppressive function of NG Tregs in a murine allotransplantation model. They used a fully major histocompatibility complex (MHC)–mismatched skin transplant model in immunodeficient mice, which were subsequently injected with the NG Tregs 3 days later. Seven days after the adoptive T cell transfer the animals were examined, the control animals showed signs of epidermal thickening and perivascular lymphocytic infiltrates, along with other signs of high grades of rejection, this included animals treated with conventional Tregs. However, the IL-2 backpack-treated animals showed attenuated signs of allograft rejection, with ~70% of the NG grafts looking healthy compared to ~30-40% in the controls animals.
The team then wanted to determine the longevity of improved allograft rejection. Here, they showed that whilst conventional Tregs treatment mean survival time of the allotransplants was ~6 days after adoptive transfer, the NG Tregs treated group had an increased allograft survival of 18 days, suggesting the new therapy could extend survival up to 3 times.
NGs promote human Treg homeostasis
Finally, the crucial question as to whether NGs could potentially translate into a clinical therapy and promote human Treg homeostasis was addressed. Here, the team used human Tregs coupled with IL-2 loaded NGs to promote the function and homeostasis of intragraft Tregs in a humanised mouse model of skin transplantation. Here, the team grafted discarded healthy human donor skin from cosmetic surgery patients onto severely immunocompromised mice – the human cells could then mount alloimmunity against the transplanted human skin grafts. Seven days later the mice were treated with Tregs. Whilst the animals given conventional Tregs showed signs of severe rejection at day 21, the NG Tregs treated group showed only mild grades of alloimmune-associated damage under the epidermis, with ~80% grafts looking healthy compared to ~40% for the conventional T cells, this suggests NG Tregs therapy warrants further investigation as an powerful new therapy for clinical translation.
Conclusion and future applications
The team here have shown that therapeutic outcomes of Treg therapy can be significantly improved by the cell surface conjugation of NGs. With respect to alloimmunity, the platform enabled the regulated spatiotemporal provision of IL-2 to antigen-primed Tregs, reducing off-target effects such a cytotoxic cell and NK cell activation. This resulted in improved graft survival, and reduced severe signs of rejection of skin transplants.
The team hope that this technology will improve the potency of adoptive Treg transfer and accelerate its translation into the clinic which has in the past been hampered in part by low levels of homeostasis of these cells. The beauty here, is this strategy can improve therapeutic outcomes without the need for genetic engineering, providing a simpler system of surface engineering – membrane-conjugate backpacks. Here, the process was achieved in less than 45 mins and was highly efficient – resulting in the conjugation of >90% of Tregs with IL-2 NGs.
The experiments here provide proof-of-concept for this system, which provides a flexible platform that can be further developed for other applications – backpacks can be loaded with alternative cargos such as other adjuvants or immunosuppressive drugs, allowing Tregs to act as living delivery systems to target payloads to certain regions and only release their freight under specific conditions. The team are planning on optimising the release kinetics from the backpacked NGs to firstly optimise the continuity of IL-2 signalling, but the finding are likely to transfer to the release of future payloads. From a safety perspective they will also being looking at off-target effects in other organs, and investigating the effectiveness of multiple doses of the therapy, which may increase longevity of immune suppression.
The ability to suppress alloimmunity and potentially autoimmunity will be a vital tool in the clinic. The key to transplantation success currently rests on suppressing the immune system with a fine balance. With this in mind, a CRISPR-based lateral flow system has been designed to detect early signs of infection and rejection following kidney transplants. One can envisage that combining this sort of low-cost simple diagnostic and monitoring assay together with backpack loaded Tregs suppression of the immune system could greatly improve long-term patient outcomes from a variety of conditions.
Eskandari, S. K., I. Sulkaj, M. B. Melo, N. Li, H. Allos, J. B. Alhaddad, B. Kollar, T. J. Borges, A. S. Eskandari, M. A. Zinter, S. Cai, J. P. Assaker, J. Y. Choi, B. S. Al Dulaijan, A. Mansouri, Y. Haik, B. A. Tannous, W. J. van Son, H. G. D. Leuvenink, B. Pomahac, L. V. Riella, L. Tang, M. A. J. Seelen, D. J. Irvine and J. R. Azzi (2020). “Regulatory T cells engineered with TCR signaling–responsive IL-2 nanogels suppress alloimmunity in sites of antigen encounter.” Science Translational Medicine 12(569): eaaw4744.
https://doi.org/10.1126/scitranslmed.aaw4744